Health
Capoeira Classes Transform Lives of Parkinson’s Patients in Brazil

A unique movement practice in Brazil is providing significant relief for patients with Parkinson’s disease. Capoeira, an art form that blends martial arts with dance, is helping individuals ease their symptoms and find community support. The classes, specifically designed for those living with the neurodegenerative condition, have gained popularity in Rio de Janeiro.
Nilma Teles de Freitas, an 80-year-old retired teacher diagnosed with Parkinson’s over a decade ago, shared her transformative experience. “Capoeira gives me freedom to work on my body. What I can do. What I can’t do. So I can have balance and a more comfortable life,” she said during a recent class held in downtown Rio.
Historical Roots and Therapeutic Benefits
Capoeira has deep historical roots, originating in the 16th century among enslaved Africans in Brazil. It combines physical exercise, music, and spirituality, and was recognized by UNESCO as an Intangible Cultural Heritage in 2014. The initiative to adapt capoeira for Parkinson’s patients began in 2018, spearheaded by Rosimeire Peixoto, a 60-year-old physical therapist.
After years of treating neurological patients, Peixoto believed that capoeira could alleviate some common symptoms of Parkinson’s, which include balance difficulties, tremors, and anxiety. “I had the idea after reading an article that said alternating both hands when using a cell phone stimulates both hemispheres of the brain,” she explained. Peixoto’s program, named “Parkinson na ginga,” translates to “Parkinson’s in the swing,” reflecting the initial fluid movements taught in capoeira.
Classes are held twice a week at the Progress Foundry, a cultural center located near an iconic 18th-century aqueduct in downtown Rio. The sessions aim to enhance balance, coordination, and strength through rhythmic movement and music, creating an engaging atmosphere for participants.
A Community of Support
During a recent class, Peixoto moved among the participants, offering gentle support and encouragement. Antônio de Azevedo, another participant diagnosed with Parkinson’s, emphasized the impact of capoeira on his stability. “It’s the best thing that’s ever happened to me,” he stated, expressing gratitude for the improvements he has experienced since beginning the practice.
Peixoto fosters a sense of community among her students, often incorporating social activities into the classes. After each session, she suggests a group samba dance and brings a cake for everyone to share.
Teles de Freitas highlighted the importance of camaraderie within the group. “We are there for one another. Feeling and conversing with friends gives strength,” she said. Reflecting on her initial diagnosis, she recalled feeling overwhelmed and fearful. “Today I’m smiling. I’m managing to live. I’m managing to interact with other people. I’m managing to be happy,” she concluded.
The capoeira classes not only provide physical benefits but also create a supportive network for individuals grappling with the challenges of Parkinson’s disease. With the combination of movement, music, and community, participants are finding renewed hope and the ability to engage with life in meaningful ways.
-

 Top Stories3 months ago
Top Stories3 months agoTributes Surge for 9-Year-Old Leon Briody After Cancer Battle
-

 Entertainment4 months ago
Entertainment4 months agoAimee Osbourne Joins Family for Emotional Tribute to Ozzy
-

 Politics4 months ago
Politics4 months agoDanny Healy-Rae Considers Complaint After Altercation with Garda
-
 Top Stories4 months ago
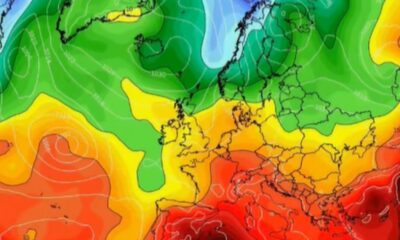
Top Stories4 months agoIreland Enjoys Summer Heat as Hurricane Erin Approaches Atlantic
-

 World5 months ago
World5 months agoHawaii Commemorates 80 Years Since Hiroshima Bombing with Ceremony
-

 Top Stories3 months ago
Top Stories3 months agoNewcastle West Woman Patricia Foley Found Safe After Urgent Search
-

 Top Stories5 months ago
Top Stories5 months agoFianna Fáil TDs Urgently Consider Maire Geoghegan-Quinn for Presidency
-

 World5 months ago
World5 months agoCouple Convicted of Murdering Two-Year-Old Grandson in Wales
-

 World5 months ago
World5 months agoGaza Aid Distribution Tragedy: 20 Killed Amid Ongoing Violence
-

 World5 months ago
World5 months agoAristocrat Constance Marten and Partner Convicted of Infant Murder
-

 Top Stories4 months ago
Top Stories4 months agoClimbing Errigal: A Must-Do Summer Adventure in Donegal
-

 Top Stories4 months ago
Top Stories4 months agoHike Donegal’s Errigal Mountain NOW for Unforgettable Summer Views









